Epidural Gas Injection (EGI) therapy uses the technique of sacral epidural anesthesia to introduce gas such as oxygen into the epidural space.
EGI was once used to treat chronic lumbago more than seventy years ago but abandoned for a long time.
We happened to find EGI is effective for chronic symptoms such as headache, vertigo, and photophobia after mild traumatic brain injury (mTBI) or whiplash injury. EGI is also effective for the autonomic dystonia such as orthostatic dysregulation (OD) and irritable bowel syndrome (IBS).
Life disturbing diseases that can be treated by Epidural Gas Injection

Epidural Gas Injection (EGI) is a treatment that employs the two procedures of air epidurography*1 and sacral anesthesia*2.
The following ailments that can be treated with EGI (which have shown significant improvement in many of the patients we have treated) are detailed below.
*1: Air epidurography: An examination method used before the advent of CT and MRI
*2: Sacral anesthesia: An anesthesia method that has been in use for over 120 years
Currently, we can list the following life disturbing diseases as the target of EGI. The patients with these diseases do not show any abnormalities on medical examinations despite their wide varieties of severe life disturbing signs and symptoms.
About 70% of the patients who received EGI returned to daily life.
Life disturbing diseases that can be treated by Epidural Gas Injection
Although the long history of the clinical and experimental research on chronic post-traumatic headache, mild traumatic brain injury, and whiplash injury, it has not yet been clearly explained why these patients have such wide varieties of severe life-disturbing signs and symptoms. We hypothesize that abnormalities in the cerebrospinal fluid dynamics and impaired function of the epidural space may take place in these disorders which be responsible for the life disturbing signs and symptoms.
How the Skull, Spinal Column, Membranes, and Cerebrospinal Fluid Protect the Brain and Spinal Cord.
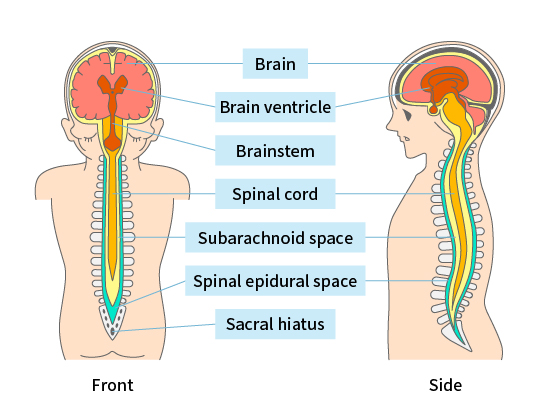
The subarachnoid space contains cerebrospinal fluid, which protects the brain and spinal cord from external damage. In the spinal canal, further outside the subarachnoid space, is the dura mater and epidural space.


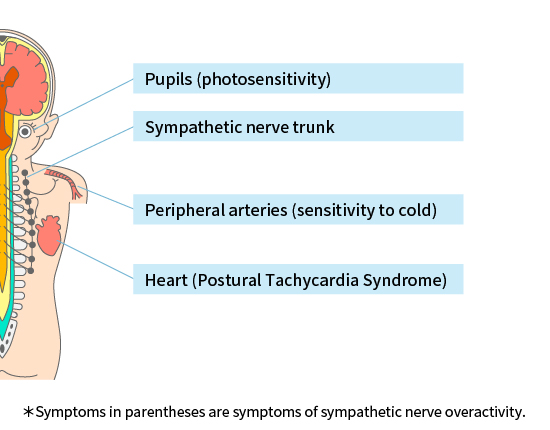
Effects of Epidural Gas Injection
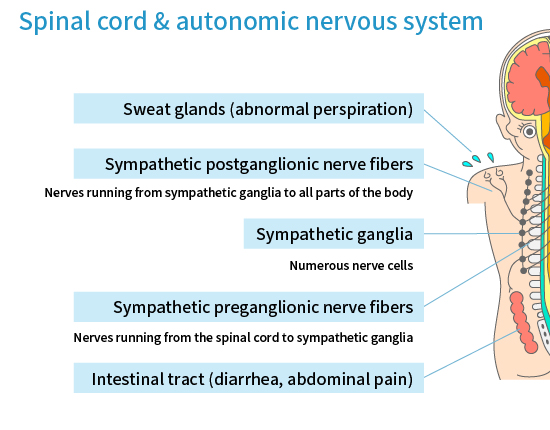
The function of the epidural space is still unclear. The epidural space contains fat tissue, lymphatic channels, and rich venous system without valves. Motor, sensory, and autonomic nerve fibers from spinal cord pass through the epidural space to the outside of the spinal column. The position of brain, spinal cord, and spinal nerves (motor, sensory, and autonomic) must be kept constant despite the change of body position (upright or recumbent). Although it has not yet been verified by the clinical and experimental studies, it is easy to imagine that the epidural space plays an important role to keep the position of brain, spinal cord, and spinal nerves constant by keeping the volume of epidural space constant. We hypothesize that any kind of damage to the epidural volume controlling system may affect the function of spinal nerves (motor, sensory, and autonomic).
The Epidural Gas Injection temporally increases the epidural pressure. Although the mechanism is not clear, this temporal increase of epidural space may normalize the epidural volume controlling system and normalize the function of nervous system.
Treatment Method
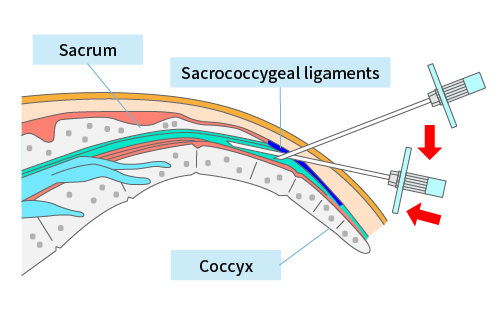
Epidural Gas Injection is a process that involves injecting a small amount of gas (air, oxygen, or helium) into the epidural space.
Treatment is performed with the patient either lying down (supine) or sitting (seated). The epidural space is punctured usually through the sacral hiatus using a lumbar puncture needle. The lumbar puncture needle used in this procedure is thinner than the epidural needle used for typical epidural punctures, so there is less risk of bleeding and much less pain. If gas tends to leak subcutaneously with this method or it is less effective, it is performed at a location between the lower thoracic and lower lumbar vertebrae. The amount of gas injected does not exceed 100ml.